Abstract
The burgeoning field of microbiota-gut-brain axis research has introduced groundbreaking perspectives on the etiology and management of Autism Spectrum Disorder (ASD). ASD's multifaceted nature, marked by diverse neurological and gastrointestinal symptoms, has long puzzled clinicians and researchers alike. Recent investigations into the bidirectional communication network connecting the enteric and central nervous systems have spotlighted the gut microbiota's pivotal role in influencing neurodevelopment and behavior. This article synthesizes current insights into the microbiota alterations in ASD, elucidates the mechanisms through which these alterations may influence the disorder, and explores novel therapeutic interventions targeting the gut microbiome.
Introduction
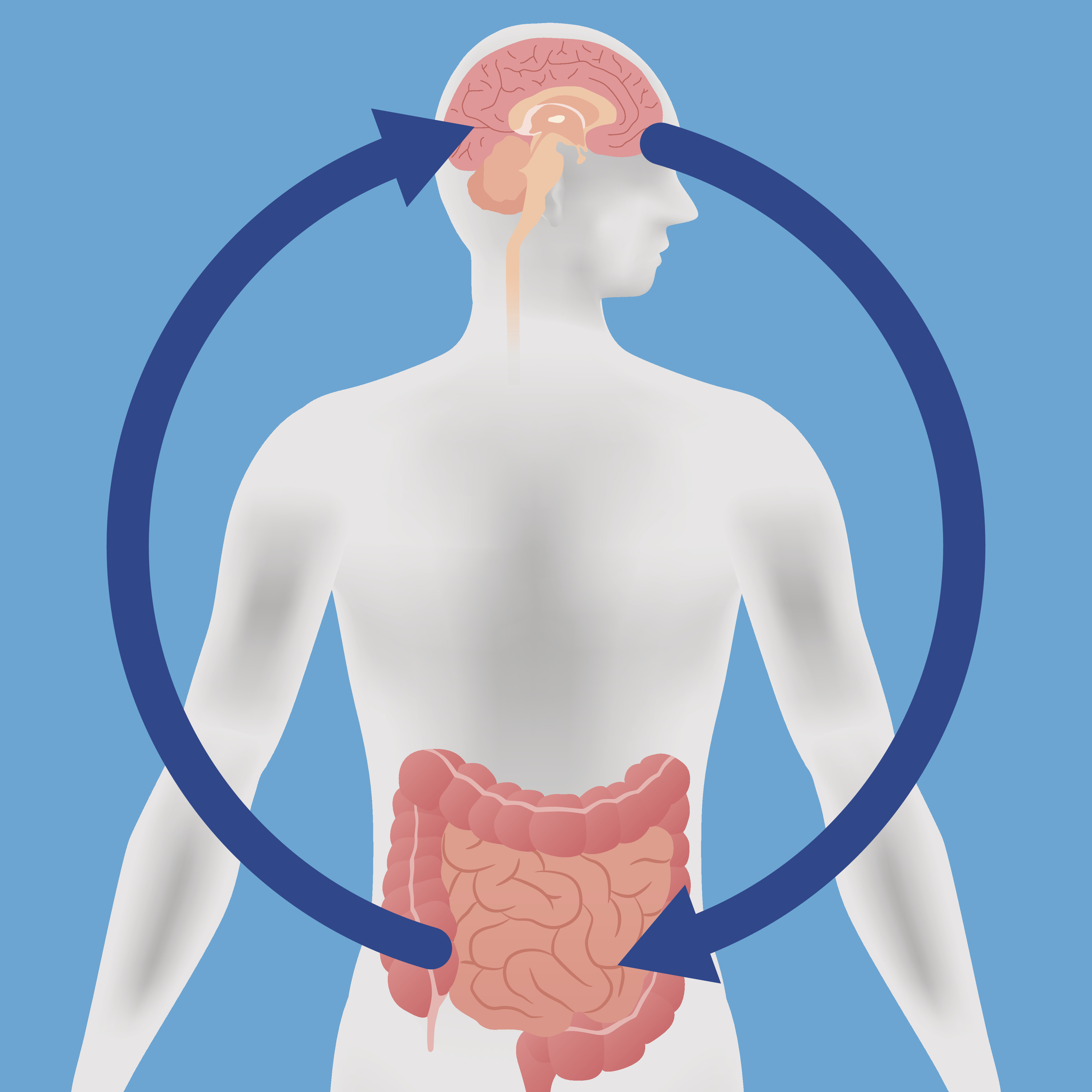
Autism Spectrum Disorder (ASD) encompasses a range of conditions characterized by challenges in social skills, repetitive behaviors, and communication difficulties, often accompanied by gastrointestinal (GI) disturbances. The intersection of neurological and GI symptoms in ASD has directed attention towards the microbiota-gut-brain axis, a complex communication network that integrates the enteric and central nervous systems through neural, hormonal, and immunological pathways. This article reviews emerging evidence of gut microbiota's influence on ASD and discusses the potential for microbiota-targeted therapies.
Microbiota Alterations in ASD
A growing body of research indicates significant microbiota composition differences in individuals with ASD compared to neurotypical controls. These alterations are not merely coincidental but are increasingly recognized as contributory to the behavioral and cognitive manifestations of ASD. The dysbiosis observed in ASD—characterized by the overrepresentation or underrepresentation of specific neuroactive compound-producing bacteria—suggests a direct link between gut microbiota and neurodevelopmental processes.
Mechanisms of Influence
Neuroactive Compound Production
Certain gut bacteria are capable of producing neuroactive compounds, such as serotonin and gamma-aminobutyric acid (GABA), which are integral to brain function and development. Altered levels of these compounds in ASD may disrupt neurodevelopmental pathways and synaptic plasticity, contributing to the disorder's symptomatology.
Immune System Modulation
The gut microbiota is essential for the proper development and functioning of the immune system. In ASD, dysbiosis can lead to immune dysregulation, characterized by chronic inflammation and altered cytokine profiles, which can adversely affect neurodevelopment and exacerbate ASD symptoms.
Gut Permeability
Increased gut permeability, or "leaky gut," observed in some ASD individuals, allows for the translocation of potentially neuroactive substances into the bloodstream. These substances can cross the blood-brain barrier, directly influencing brain function and contributing to the neurological symptoms of ASD.
Therapeutic Implications
The gut microbiota's role in ASD opens new avenues for therapeutic interventions. Dietary modifications, probiotic supplementation, and fecal microbiota transplantation (FMT) are explored as strategies to modulate the gut microbiome, offering potential improvements in ASD symptoms.
- Dietary Modifications: Specific diets that promote beneficial gut bacteria or reduce harmful ones have shown promise in symptom improvement, highlighting the therapeutic potential of dietary interventions.
- Probiotic Supplementation: Targeted probiotic strains may help restore a healthy microbial balance, with preliminary studies reporting symptom improvements in ASD individuals.
- Fecal Microbiota Transplantation (FMT): Although experimental, FMT has shown potential in reconstituting gut microbiota and improving gastrointestinal and certain behavioral symptoms in ASD, underscoring the profound impact of gut microbiota on neurological health.
Conclusion
The exploration of the microbiota-gut-brain axis in ASD offers a novel perspective on the disorder's underlying mechanisms and potential treatment strategies. By focusing on the intricate relationships between gut microbiota, immune responses, and brain function, this research illuminates promising pathways for developing targeted interventions. Future studies will be crucial in further unraveling these complex interactions and translating them into effective treatments, potentially transforming the management of ASD and improving the lives of affected individuals and their families.